Arthritis, Degeneration, Fractures and Pain: part, but not all, of the problem
Arthritis, osteoarthritis, spondylosis and bony degeneration are terms used interchangeably to describe the wear-and-tear degradation of the portion of a bone facing a joint. A joint is where two bones meet. The spine, with its hard bone vertebrae separated by the cushions of the intervertebral disks, has many joints. Where bones form a join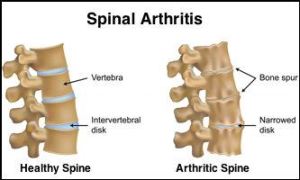 t, there is softer cartilage surface that responds to mechanical challenge by producing new bone. Mechanical pressure (standing, walking, sitting, running) destroys a very small number of bone cells. This destruction signals new bone to form in response to injury. As we age, this process may either not “keep up” with our daily “wear-and-tear” (thinning, “bone-on-bone” arthritis), or may actually over-respond, producing extra bone growth, like that of a bunion, called an osteophyte or bone spur. When this process occurs at the back/side portion of the vertebrae/spine, where the nerve roots exit the spinal cord, this is called facet arthritis/arthropathy/syndrome.
t, there is softer cartilage surface that responds to mechanical challenge by producing new bone. Mechanical pressure (standing, walking, sitting, running) destroys a very small number of bone cells. This destruction signals new bone to form in response to injury. As we age, this process may either not “keep up” with our daily “wear-and-tear” (thinning, “bone-on-bone” arthritis), or may actually over-respond, producing extra bone growth, like that of a bunion, called an osteophyte or bone spur. When this process occurs at the back/side portion of the vertebrae/spine, where the nerve roots exit the spinal cord, this is called facet arthritis/arthropathy/syndrome.
In the first two decades of life, 80 to 90 percent of the weight of the lower back spine is distributed across the back one-third of the disk: the portion where nerve roots exit. The disks have a high water content, and shrink with age. As the disks shrink, the bony facet joints start to bear the weight formerly borne by the disks, and the bone experiences more mechanical stress than earlier in life. As these bony changes take place, muscles begin to pull in new ways, possibly causing or compounding the low back pain seen with arthritis. If a bone spur happens to form in this region, it may irritate a nerve root leaving the spine, producing sciatica.
Although we often assume degenerative conditions of the spine (arthritis, facet joint syndrome) and disks (DDD) cause pain, controlled studies indicate minimal-to-no correlation between pain symptoms and radiological signs of degeneration [16, 18-23]. Other clinical research reports facet joint findings in 15 to 45 percent of patients with LBP. Some still argue that the bony changes of arthritis are responsible for its pain, others believe the bony changes pulling on soft tissues cause pain. Either way, arthritis pain is usually relatively mild: morning stiffness resolving with the day’s activities, occasionally referring pain to the upper/mid back and/or lower legs. Conventional treatment includes medications, physical therapy and daily exercise. Surgery is sometimes required if bone spurs impact neurological functioning.
Some arthritic and thin (osteoportic) bone can fracture later in life, resulting in vertebral compression fractures. Medications, back bracing, and some novel injections of cement-type substances are being tried to help this significant cause of chronic pain.
X
1 Anderssen GBJ. Frymoyer JW (ed.). The epidemiology of spinal disorders, in The Adult Spine: Principles and Practice. New York: Raven Press; 1997:93-141.
2 Cunningham LS, Kelsey JL. Epidemiology of musculoskeletal impairments and associated disability. Am J Public Health. Jun 1984;74(6):574-9. [Medline].
3 National Center for Health Statistics (1977):. Limitations of activity due to chronic conditions, United States. Series 10, No.111. 1974..
4 National Center for Health Statistics (1975):. Physician visits, volume and interval since last visit, United States. 1971. Series 10, No.97.
5 Nachemson Al, Waddell G, Norland AL. Nachemson AL, Jonsson E (eds.). Epidemiology of Neck and Low Back Pain, in. Neck and Back Pain: The scientific evidence of causes, diagnoses, and treatment. Philadelphia: Lippincott Williams & Wilkins; 2000:165-187.
6 Mayer TG, Gatchel RJ. Functional restoration for spinal disorders: The sports medicine approach. Philadelphia: Lea & Febiger; 1988.
7 Biering-Sorenson F. Low back trouble and a general population of 30-, 40-, 50-, and 60–year-old men and women. Dan Med Bull. 1982;29:289-99.
8 Damkot DK, Pope MH, Lord J, Frymoyer JW. The relationship between work history, work environment and low-back pain in men. Spine (Phila Pa 1976). May-Jun 1984;9(4):395-9. [Medline].
9 “Acupuncture Energetics: A Clinical Approach for Physicians”. Joseph M. Helms. Medical Acupuncture Publishers; 1st Edition. (1995)
10 “Foundations of Chinese Medicine: A Comprehensive Text for Acupuncturists and Herbalists”. Giovanni Maciocia. Churchill Livingstone; 2 Edition (July, 2005).
11 “Travell & Simons’ Myofascial Pain and Dysfunction: The Trigger Point Manual”. David G. Simons, Janet G. Travell, Lois S. Simons, Barbara D. Cummings. Lippincott Williams & Wilkins; 2 edition (1998)
12 “Traditional Chinese Medicine Cupping Therapy”. Ilkay Chirali. Churchill & Livinstone; 2 editioin (2007)
13 Argoff CE, Wheeler AH. Backonja MM, ed. Spinal and radicular pain syndromes. Philadelphia, WB Saunders: Neurologic Clinics; 1998:833-45.
14 Wheeler AH. Diagnosis and management of low back pain and sciatica. Am Fam Physician. Oct 1995;52(5):1333-41, 1347-8.
15 Wheeler AH, Murrey DB. Spinal pain: pathogenesis, evolutionary mechanisms, and management, in Pappagallo M (ed). The neurological basis of pain. New York: McGraw-Hill; 2005:421-52.
16 “Essentials of Musk Care”
17 Mooney V. Presidential address. International Society for the Study of the Lumbar Spine. Dallas, 1986. Where is the pain coming from?. Spine (Phila Pa 1976). Oct 1987;12(8):754-9. .
18 Waddell G. 1987 Volvo award in clinical sciences. A new clinical model for the treatment of low-back pain. Spine (Phila Pa 1976). Sep 1987;12(7):632-44.
19 Frymoyer JW. Back pain and sciatica. N Engl J Med. Feb 4 1988;318(5):291-300.
20 Argoff CE, Wheeler AH. Backonja MM, ed. Spinal and radicular pain syndromes. Philadelphia, WB Saunders: Neurologic Clinics; 1998:833-45.
21 Mooney V. Presidential address. International Society for the Study of the Lumbar Spine. Dallas, 1986. Where is the pain coming from?. Spine (Phila Pa 1976). Oct 1987;12(8):754-9.
22 Wheeler AH, Hanley EN Jr. Nonoperative treatment for low back pain. Rest to restoration. Spine (Phila Pa 1976). Feb 1 1995;20(3):375-8. [Medline].
23 Jensen MC, Brant-Zawadzki MN, Obuchowski N, Modic MT, Malkasian D, Ross JS. Magnetic resonance imaging of the lumbar spine in people without back pain. N Engl J Med. Jul 14 1994;331(2):69-73