For Spinal Stenosis, click here
An estimated 4.1 million Americans had symptoms of an intervertebral disk disorder between 1985 and 1988, and, of those, as many as 60 percent of men 45 years or older reported having sciatica. Sciatica leads to surgery more often than does back pain alone.
Intervertebral disks lie between the bones of the spine (vertebrae), and function as shock absorbing cushions between the vertebrae. Every time you walk, run, bend, lift, twist (etc), force travels to and through the spine. The spine’s function is to protect the delicate spinal cord, the large nerve which functions as the main “cable of communication” from the brain to the rest of your body. [15,16]
The disks are round, doughnut-like structures that have two pieces: a tough, outer ring (annulus fibrosus) that contains a soft center (nucleus pulposus) with a high water content, about the consistency of toothpaste. Spinal injury and/or wear and tear (twisting, flexing, extending, repeated loading) may cause the outer ring to tear. When this occurs, the soft center “pop outs” or “herniates” through the tough outer ring. Because the soft, toothpaste-like nucleus pulposus is not supposed to be outside of the ring, it produces inflammation in the area of either the spinal cord or nerve roots, which irritates these nerves.
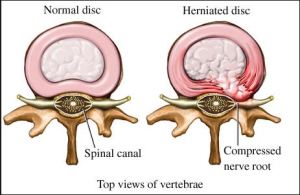
If you look at the diagram above, you can see that the spine has a canal in the center where the spinal cord is. The spinal canal and cord are in the center of the spine. Additionally, there are holes toward the back and sides of the vertebral bones, where nerve roots leave to connect the spinal cord/brain to the rest of the body. For example, some nerve roots travel to legs/foot to signal them to move, others sense pain. This aspect of the spine faces toward the sides/back of the body.
When the disk ring partially tears, the soft nucleus pops out either toward the center (the spinal cord) or toward the back/sides (the nerve roots). Disk herniation producing nerve root irritation is one way sciatica occurs. Much less commonly, the disk herniates toward the center/spinal cord, producing problems with leg movement or, rarely, cauda equina syndrome (see below).[16] Even less commonly, the disk’s outer ring acutely and completely ruptures, requiring immediate surgery (disk rupture).
Normal, healthy disks do not sense pain, as they do not have pain-sensing nerves in them. However, badly damaged disks do obtain these these “pain sensors” over time (this also occurs with degenerative disk disease). Therefore, healthy, torn disks do not produce pain; it is the disk material and its associated inflammation that signal pain. As a result, most disk herniations will respond/resolve with time and/or physical therapy to help stabilize the spine and prevent recurrence. Conventional therapy also includes non-steroidal anti-inflammatories, anti-inflammatory steroids, narcotics, muscle relaxants, epidural injections with steroid, and occasionally surgery (microdiskectomy or diskectomy with laminectomy).[16]
The rare, significant, sudden form of central disk herniation called cauda equina syndrome, commonly produces pain in one leg, paralysis of the legs (without spasticity), bowel and bladder changes (incontinence or retention), as well as “saddle anesthesia:” a numbness or tingling in the crotch area that may extend to the interior of the upper thighs. There is weakness when transferring from sitting to standing and with heel/toe walking. This is an urgent condition and must be immediately evaluated by a surgeon.
X
1 Anderssen GBJ. Frymoyer JW (ed.). The epidemiology of spinal disorders, in The Adult Spine: Principles and Practice. New York: Raven Press; 1997:93-141.
2 Cunningham LS, Kelsey JL. Epidemiology of musculoskeletal impairments and associated disability. Am J Public Health. Jun 1984;74(6):574-9. [Medline].
3 National Center for Health Statistics (1977):. Limitations of activity due to chronic conditions, United States. Series 10, No.111. 1974..
4 National Center for Health Statistics (1975):. Physician visits, volume and interval since last visit, United States. 1971. Series 10, No.97.
5 Nachemson Al, Waddell G, Norland AL. Nachemson AL, Jonsson E (eds.). Epidemiology of Neck and Low Back Pain, in. Neck and Back Pain: The scientific evidence of causes, diagnoses, and treatment. Philadelphia: Lippincott Williams & Wilkins; 2000:165-187.
6 Mayer TG, Gatchel RJ. Functional restoration for spinal disorders: The sports medicine approach. Philadelphia: Lea & Febiger; 1988.
7 Biering-Sorenson F. Low back trouble and a general population of 30-, 40-, 50-, and 60–year-old men and women. Dan Med Bull. 1982;29:289-99.
8 Damkot DK, Pope MH, Lord J, Frymoyer JW. The relationship between work history, work environment and low-back pain in men. Spine (Phila Pa 1976). May-Jun 1984;9(4):395-9. [Medline].
9 “Acupuncture Energetics: A Clinical Approach for Physicians”. Joseph M. Helms. Medical Acupuncture Publishers; 1st Edition. (1995)
10 “Foundations of Chinese Medicine: A Comprehensive Text for Acupuncturists and Herbalists”. Giovanni Maciocia. Churchill Livingstone; 2 Edition (July, 2005).
11 “Travell & Simons’ Myofascial Pain and Dysfunction: The Trigger Point Manual”. David G. Simons, Janet G. Travell, Lois S. Simons, Barbara D. Cummings. Lippincott Williams & Wilkins; 2 edition (1998)
12 “Traditional Chinese Medicine Cupping Therapy”. Ilkay Chirali. Churchill & Livinstone; 2 editioin (2007)
13 Argoff CE, Wheeler AH. Backonja MM, ed. Spinal and radicular pain syndromes. Philadelphia, WB Saunders: Neurologic Clinics; 1998:833-45.
14 Wheeler AH. Diagnosis and management of low back pain and sciatica. Am Fam Physician. Oct 1995;52(5):1333-41, 1347-8.
15 Wheeler AH, Murrey DB. Spinal pain: pathogenesis, evolutionary mechanisms, and management, in Pappagallo M (ed). The neurological basis of pain. New York: McGraw-Hill; 2005:421-52.
16 “Essentials of Musk Care”
17 Mooney V. Presidential address. International Society for the Study of the Lumbar Spine. Dallas, 1986. Where is the pain coming from?. Spine (Phila Pa 1976). Oct 1987;12(8):754-9. .
18 Waddell G. 1987 Volvo award in clinical sciences. A new clinical model for the treatment of low-back pain. Spine (Phila Pa 1976). Sep 1987;12(7):632-44.
19 Frymoyer JW. Back pain and sciatica. N Engl J Med. Feb 4 1988;318(5):291-300.
20 Argoff CE, Wheeler AH. Backonja MM, ed. Spinal and radicular pain syndromes. Philadelphia, WB Saunders: Neurologic Clinics; 1998:833-45.
21 Mooney V. Presidential address. International Society for the Study of the Lumbar Spine. Dallas, 1986. Where is the pain coming from?. Spine (Phila Pa 1976). Oct 1987;12(8):754-9.
22 Wheeler AH, Hanley EN Jr. Nonoperative treatment for low back pain. Rest to restoration. Spine (Phila Pa 1976). Feb 1 1995;20(3):375-8. [Medline].
23 Jensen MC, Brant-Zawadzki MN, Obuchowski N, Modic MT, Malkasian D, Ross JS. Magnetic resonance imaging of the lumbar spine in people without back pain. N Engl J Med. Jul 14 1994;331(2):69-73